The Pain Response–New Ways of Thinking
Without a shadow of a doubt, the modern-day circus artist is exposed to high training loads and increasingly competitive and saturated performance calendars. Injuries from circus training and pain associated with them often lead to the inability to train or perform causing physical, emotional and financial stressors.
If the pain response is better understood by circus practitioners, we strongly believe that you can take action to manage it and move forward more successfully.
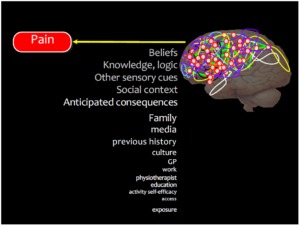
Nobody experiences pain as you do. Your pain experience is individual. It is manufactured by your brain using a variety of inputs namely, proprioception (information from different parts of the body) and cognition (beliefs, memory, feelings, logic).
The most important take-away from this blog post is to make you aware that there are many factors that govern your pain response. It’s not a simple electric circuit.
This article’s aim is to shed some light on the advances in modern day pain physiology which can help diminish the sense of threat for circus artists.

How Do We Interpret Pain? Challenging the Traditional Paradigm
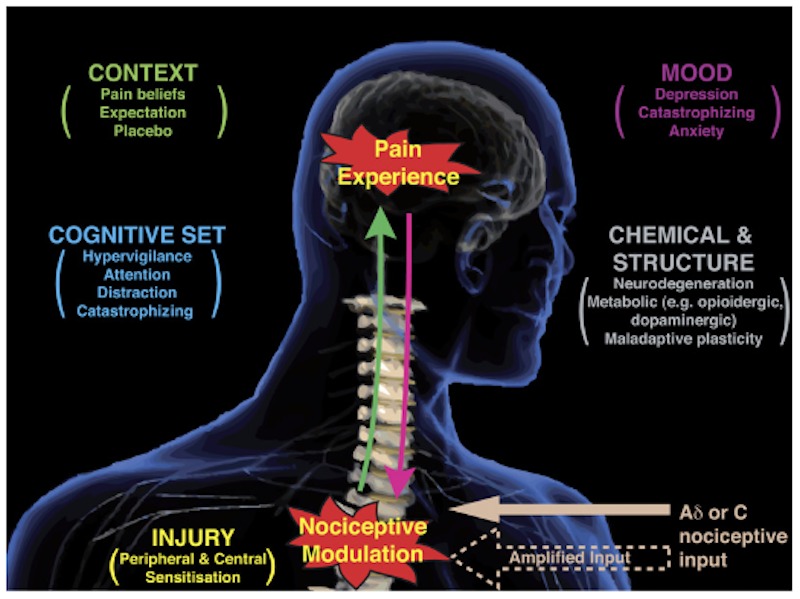
Before we actually experience a painful sensation, the brain has to make a detailed calculation: do I need to give this circus person a warning of some kind to ensure they don’t injure themselves or cause further damage on an existing injury?
Let’s break down (and simplify) how the body tackles this complex algorithm: Let’s imagine you’re training aerial straps at an intermediate level and you’ve just introduced side planche practice. Nerve fibres from your shoulder send messages to your brain about the position of all your body parts, if they are controlled and well balanced. This includes information such as physical load, pressure, velocity of stretch, thermal, mechanical and chemical condition of the tissues. The transition into side planche might be sufficiently intense to activate free nerve endings – traditionally (but not quite right) understood as danger receptors – but also those general information receptors, in a way that they can end up becoming nociceptors (receptors for potential damage). Both work together on providing information about location and the qualities of the stimulus. A ‘your shoulder is in potential danger’ message is sent to the spinal cord and up to the brain.
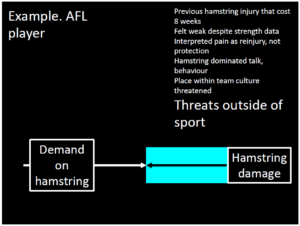
The brain has to make a judgement call about just how dangerous this actually is (as shoulder pain may have occurred frequently when training straps in the past). The brain makes fast calculations based on historical events and context.
Brain poses the question:
“Is it just the same type and intensity of pain I usually get when I train straps?”
The brain formulates an answer by processing the information gained from nerve receptors and also from cognition:
“This pain reminds me of when I almost dislocated my shoulder last year….I remember my friend having a dislocation doing this last month…My physical therapist also said I was too weak to train this move…Conclusion: This looks like a threat and could be really dangerous, I’ll make it HURT really bad so I protect it!!”
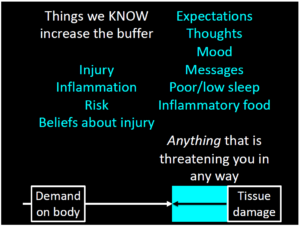
The brain has concluded that it’s best to trigger pain in this situation expecting you to take action, because the shoulder could potentially suffer further damage. We must not forget that under inflammatory situations (general, eg.: being overstressed, sleeping poorly, etc) or localized injury, (eg.: sprained ankle, shoulder impingement, etc.) the system tends to overprotect, generating increased nociceptive information as a protective buffer.
Now here’s the really interesting part: We can all agree that the pain response is an output of your brain designed to protect you. However, what you may not know is that the pain doesn’t actually come from your shoulder – it’s the brain that projects the illusion that pain exists there. Wait, what?
Let’s pause to think about this for a minute. What we are saying is that pain is a construct of your brain.
That being said, we’re not trying to say that your ‘pain is all in your head’ and that you should ignore it. The take home message is that pain is experienced and felt at different intensities and nuances according to several other factors including: beliefs, thoughts, knowledge, feelings, friends, colleagues, community, culture, inflammation, tissue pathology, genetics and many more factors.
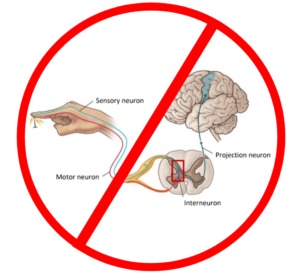
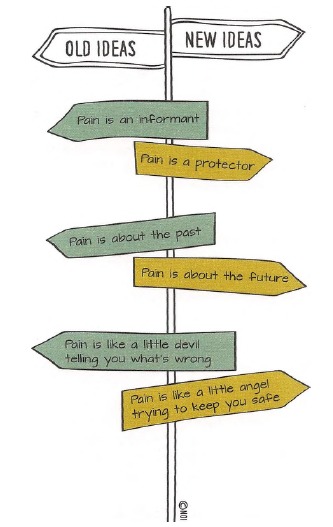
Out With Pain Pathways and in With Neurotags
The good ol’ days, when we all believed (doctors included) in the idea that there is a “pain pathway” that carries the messages from the “pain receptors” located in different parts of your body to your brain is very inaccurate. It is an outdated paradigm for understanding pain.
Traditional Pain Pathway Model
If this old paradigm were true, we could just cut those dastardly pathways and make the pain disappear — but we can’t. In fact, health economists have estimated an annual cost of treating pain at $635 billion a year, which is more than the yearly costs for cancer, heart disease and diabetes.
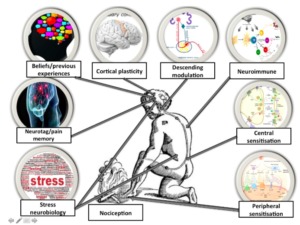
In order to understand how pain really works, we must radically change the long held beliefs about it. Since the neuromatrix theory proposed by Melzack in 1990, we became aware that pain actually works as a distributed process, where brain cells work in parallel, forming networks that stretch across multiple areas of the brain. These networks have been renamed more recently as neurotags.
This game change concept is actually great news as we have an “in”–an opportunity to influence these neurotags and modulate how we perceive and relate to pain.
Neurotags – What Are They?
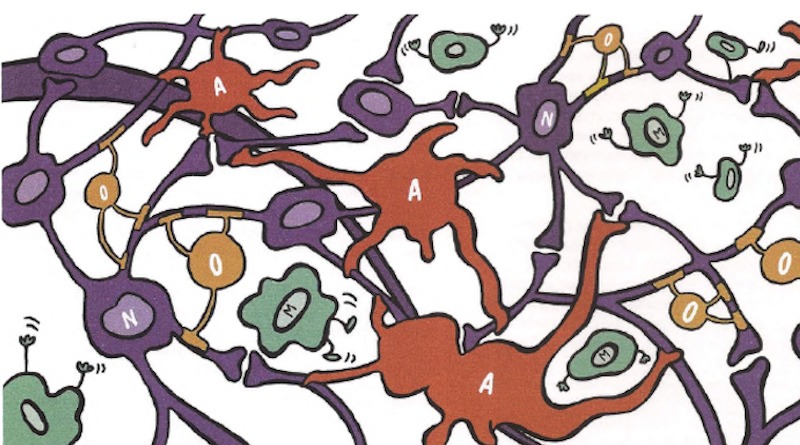
Neurotags in a nutshell refer to the pattern of neurone activation in the brain, which produces an output. It refers to the idea that networks of large groups of brain cells, distributed around the brain, work in synergy to produce outputs. They are not only made of neurons (nerve cells), but also (and mostly) by immune system cells. So in effect, our brain is a mass of these heavily intertwined cells ready to jump into action over any sign of attack.
Glia or glial cells (Greek for glue), account for 90 percent of the brain’s cells and more than half of its volume, outnumbering neurons by a ratio of 10:1. They have numerous functions, but mainly they act to hold the neurons together, provide them with nutrients and to protect them from attack. That’s why nowadays it’s more accurate to describe the nervous system as a neuroimmune system. This leads us to our next point.
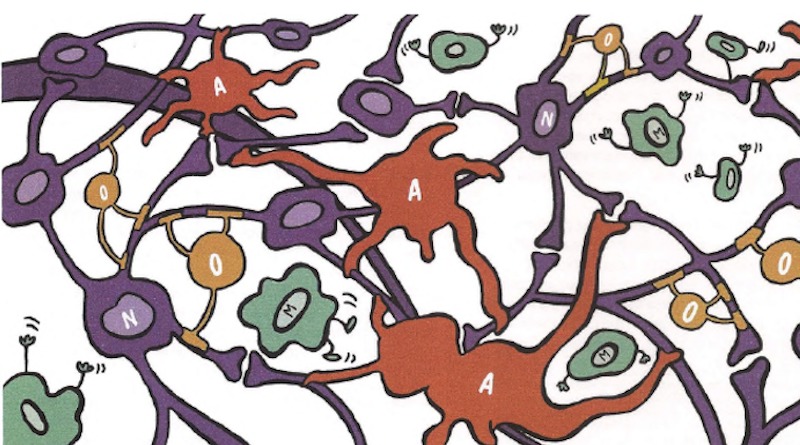
This intricate net of neurons and glial cells are wired in a way that they can exert influence and be influenced by nearby cells, that are not necessarily part of the same neurotag.
How Neurotags Can be Formed
Cells of one neurotag can also be shared by another neurotag. Let’s imagine you just visited the hospital and were just diagnosed with a hernia in your lumbar spine. You look at the MRI together, see the black protruding disc and the spinal surgeon explains in great detail, all of the unpleasant possible signs and symptoms that might relate to this diagnosis. On the way home you see an old man walking in a really poor way with his hands over the lumbar spine. Next day, when you get to the training facility and comment with some friends about it, they make jokes and are not very sympathetic about your situation. Each experience adds to your fear and creates multiple neurotags to feed into a potential pain response. The surgeon neurotag (things you hear), the old man neurotag (things you see) and the friends neurotag (people in your life). For each of them, there is a neurotag that is created, linked to each other by association through neuronal connection or glial influence. They can all modulate pain, it all depends on how they affect each one of us, by up or down-regulating the perceived threat.
In essence, cells collaborate to form neurotags. Single cells by themselves are not capable of doing much, but when they interact with other cells they can exert varying degree of influence depending on the size of the neurotag, its synaptic efficiency and its precision.
So Pain Doesn’t Just Come From the Injured Body Part?
Correct! It’s highly likely that contributors to pain may vary from day to day, and potentially from moment to moment. We are so-called ‘bioplastic creatures’. There are factors that both increase and decrease our pain experience.
To increase your awareness of the factors that can possibly affect your pain, Lorimer Mosley and the NOI group have created a practical device using two categories of neurotags DIMs (danger in me) and SIMs (safety in me).
The more DIMs you have, the greater the risk of hitting the pain threshold, and the more SIMs you have, the lower the risk of hitting the pain threshold. An example of a DIM is receiving a diagnosis of ‘disc prolapse’; an example of a SIM is spending a good time with friends. They both respond to things you hear, see, smell, taste, touch. Things you do, things you say, things you believe, places you go, people in your life, things happening in your body. You can generate two columns called a Protectometer, working a lot like a pain thermometer.
Try to do this exercise right now. If you are experiencing pain, try to write down everything that might be influencing your pain. It’s sometimes quite hard to find where DIMs and SIMs are, especially if you haven’t ever thought about it deeply.
So now we have information about what might be modulating your pain, how can you use this to your benefit?
Remember the formula:
Pain = DIMs – SIMs
SIMs are every sort of stimulus that might increase your sensation of safety related to a pain process. Things like pain education, feeling supported by the loved ones, updated health professionals, and multimedia material about pain management allow us to rethink and decrease our fear about moving, and movement is one of the best pain management tools.
Do not get it wrong, pain does tell us that there might be potential injury in the tissue, but be specially suspicious if the tissue is the main (or only) concern with insisting pain patterns, mainly with the ones that you have treated and respected healing time. There might be many other issues playing a role in this pain equation.
This article is not medical advice. If you are experiencing any pain or illness, we recommend you see a healthcare professional, preferably an up to date one.
To Summarise
- Pain is an unpleasant feeling that is felt somewhere in the body and urges us to protect that bodily location.
- Pain is one of many protective mechanisms. Others might include movement, immune, cognitive, endocrine and autonomic.
- Pain is the only protective mechanism we are necessarily aware of and compels us to do something to protect the painful bit.
- Pain is modulated by any credible evidence that protection is warranted.
References: DeLeo, J. A. (2006). Basic Science of Pain. The Journal of Bone and Joint Surgery (American), 88(suppl_2), 58. Butler,DS;MoseleyGL. Explain Pain Supercharged. Adelaide City West∫ NOI Group. Publications,2017. 3.Irene Tracey & Patrick W. Mantyh. The Cerebral Signature for Pain Perceptionand and its Modulation, 2007. Moseley, L. Modern Pain Science Workshop - London, 2019. Rio, E., Moseley, L., Purdam, C., Samiric, T., Kidgell, D., Pearce, A. J., … Cook, J. (2013). The Pain of Tendinopathy: Physiological or Pathophysiological? Sports Medicine, 44(1), 9–23.
All photos courtesy of James Wellington & Daniel Nogueira
Editor's Note: At StageLync, an international platform for the performing arts, we celebrate the diversity of our writers' backgrounds. We recognize and support their choice to use either American or British English in their articles, respecting their individual preferences and origins. This policy allows us to embrace a wide range of linguistic expressions, enriching our content and reflecting the global nature of our community.
🎧 Join us on the StageLync Podcast for inspiring stories from the world of performing arts! Tune in to hear from the creative minds who bring magic to life, both onstage and behind the scenes. 🎙️ 👉 Listen now!